The Challenge
- Yet, data produced for each neonate is not captured and presented as actionable information
- Leaving care teams to manually sort and evaluate mountains of data in order to respond with timely interventions
- Resulting in adverse medical outcomes, human error and care team burnout.
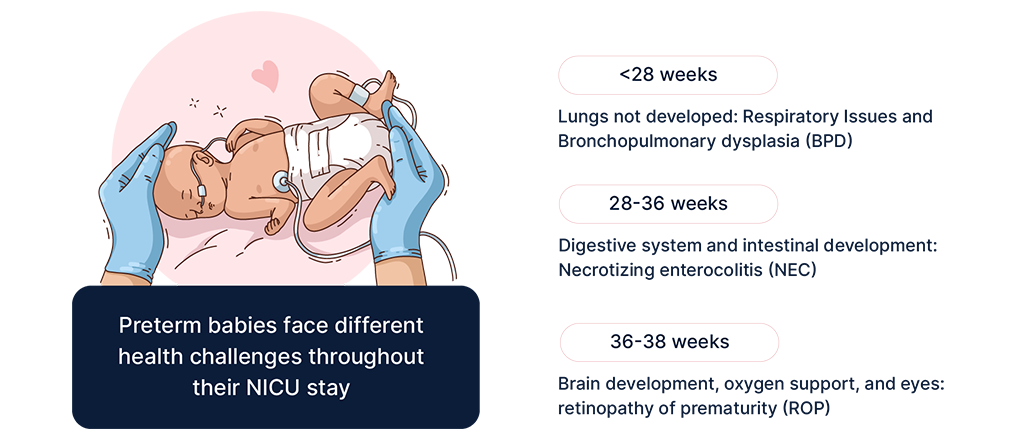
Every neonate in the NICU is highly vulnerable to rapid declines in viability
The earlier the baby is born before its normal due date, the more vulnerable the baby is. Preterm infants are at substantially higher risk for a variety of immediate as well as long term health problems including; blindness, hearing loss, sepsis, cerebra palsy, impaired learning, sudden infant death syndrome and other behavioral and psychological problems. This is, in part due to complications that lead to preterm birth but also, and more significantly, it relates to the neonate’s interrupted development. During the final weeks of pregnancy, major growth and development takes place in key organs (including skin, lungs, eyes and digestive tract).
Key Issues facing NICU care teams
The major challenge facing NICU medical staff is monitoring for warning signs and responding with timely and appropriate interventions.
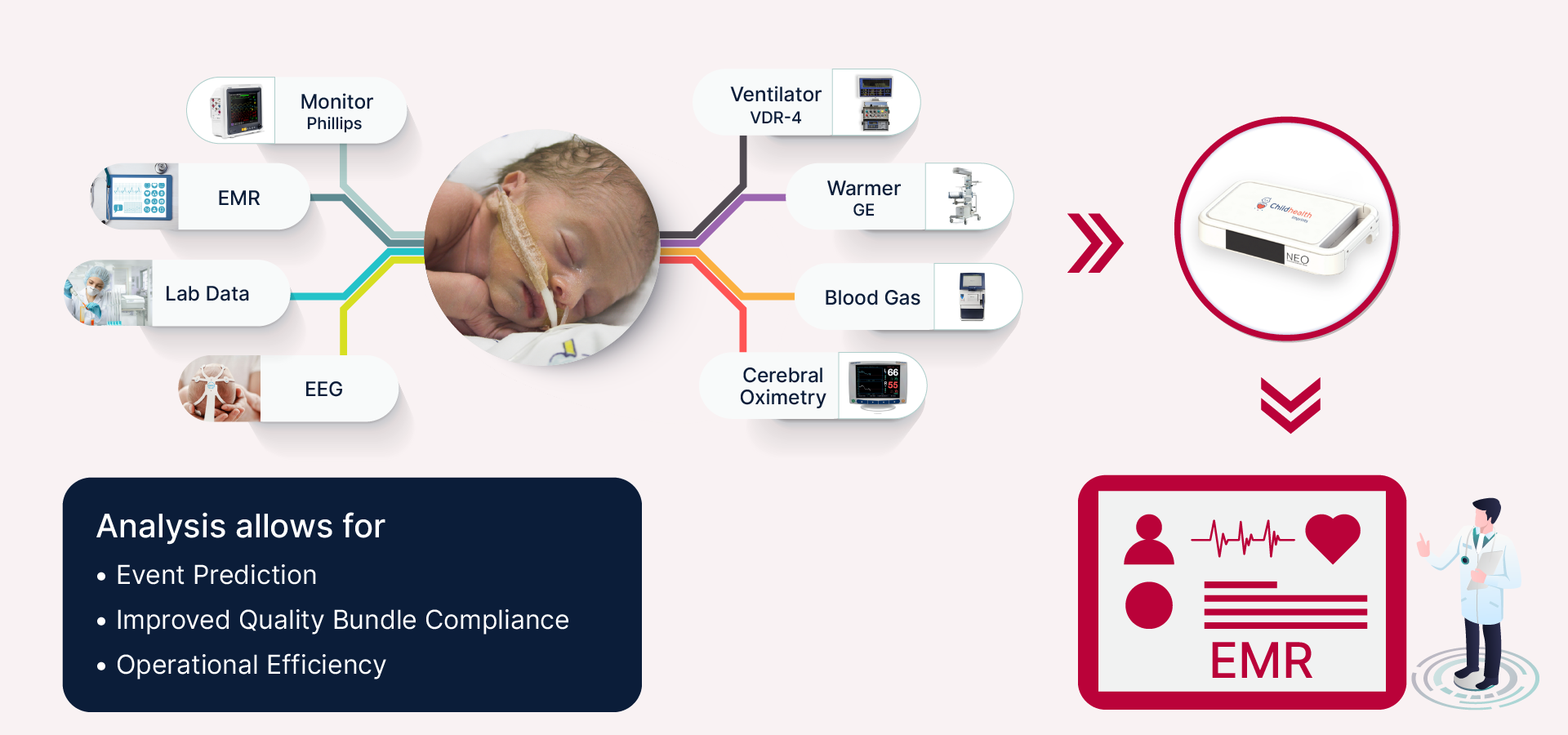
To facilitate care, NICUs are equipped with sophisticated instrumentation that tracks each neonate real time across many indicators such as ventilator data, body temperature, heart rate, EEG, blood oxygen, and more. These devices stream gigabytes of data daily in the NICU which must be assimilated by the care team to enable any needed action. Yet the care teams must rely on manually surveilling the data flows in order to respond to changing condition.
The result is human error, missed interventions and lack of timely response to warning signs all putting the infant’s health at risk while adding to staff stress and reducing efficiency.
Why are NICUs still manually trying to manage this data?
NICUs are ripe for a cutting edge data science solution to improve care and optimize operations. The data is already being collected. What is missing is a platform that captures the data and applies advances in data analytics, machine learning and artificial intelligence to provide care teams with the decision support needed to respond with informed timely decisions.
While data analytics uses proliferate, NICUs are mostly unchanged from a decade ago
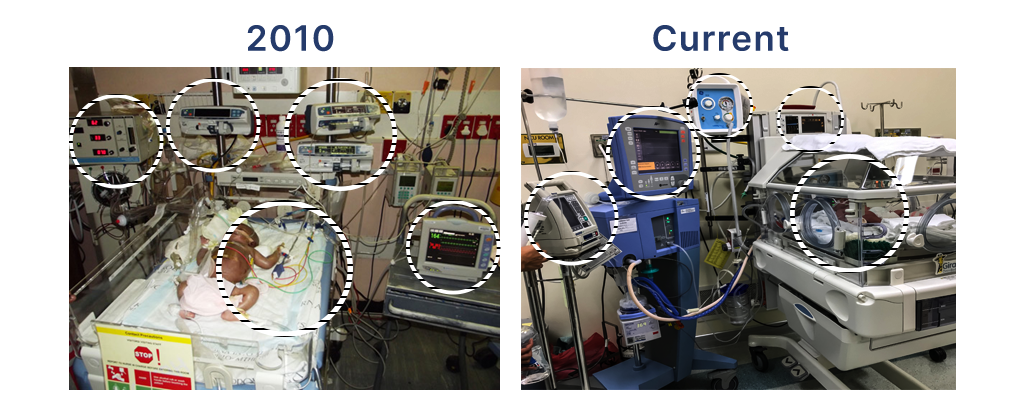
Data Science has already transformed other sectors in healthcare
Over the last several years progress in applying data science to healthcare has resulted in the emergence of medical decision support systems that leverage computing capabilities by capturing raw data streams and then storing, organizing, recalling and presenting actionable information in real time to enable doctors and nurses to make decisions about treatments and interventions. Advances in technology and digitization of information has led to the ability to construct rich datasets containing text, images, audio, video and charts. Advent of IoT, machine learning and AI further enables pattern and trend recognition which have become valuable in helping doctors and nurses understand changing factors in patients’ condition, spot potential adverse outcomes early and avoid unintended consequences they may have missed otherwise.
It is clear that data-enabled health care has already saved countless lives across the entire range of healthcare.
Today’s NICU’s need a data-enabled clinical decision support system that solves core problems faced today